- BY Kevin Barry BSc(Hons) MRICS
- POSTED IN Latest News
- WITH 0 COMMENTS
- PERMALINK
- STANDARD POST TYPE

Introduction: A Single Island Standard of Care — Linking Option B, the Bengoa Vision, and the Strangford Lough Crossing
Northern Ireland’s health system stands at the same crossroads the Bengoa Report (2016) identified:
too many hospitals, stretched rotas, inconsistent outcomes, and unsustainable duplication.
Eight years on, the fundamental message remains valid — safety and sustainability require networks, not nostalgia.
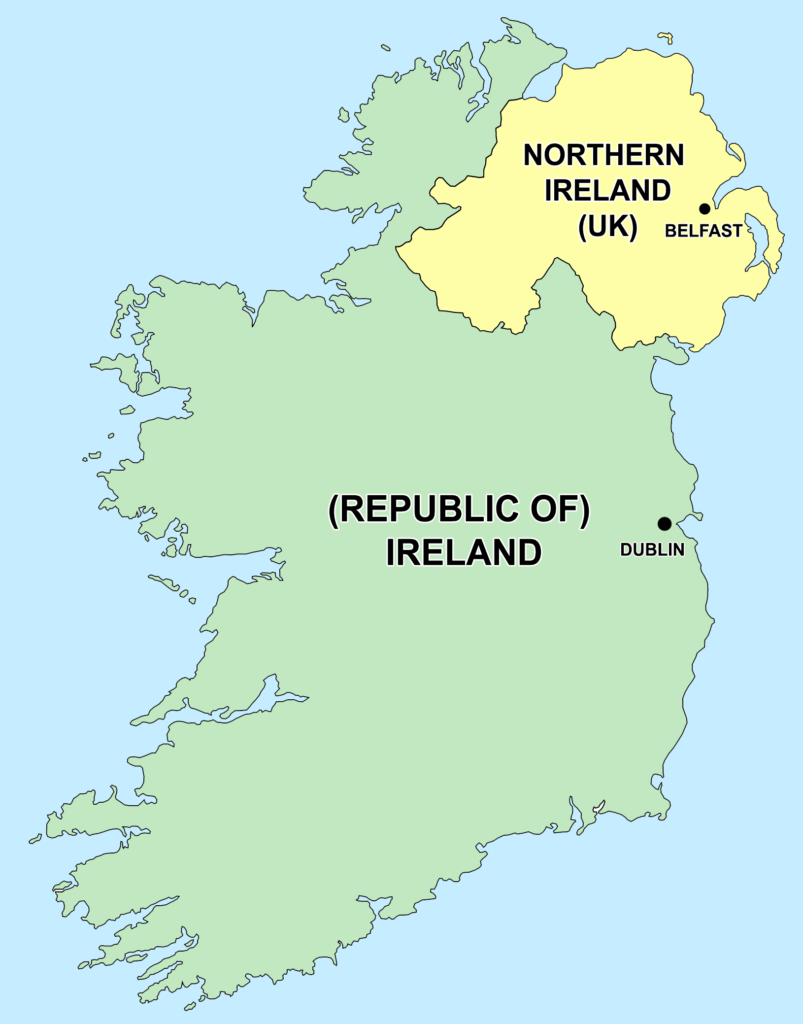
Option B, our proposed All-Island Convergence Model, applies that logic across the island of Ireland. It does not merge budgets or politics, but it sets a common patient standard:
“Every person, north or south, should be within one hour of a full acute hospital, supported by shared specialist and elective centres.”
Under this framework, Northern Ireland retains nine full 24/7 acute hubs, including the Ulster, Craigavon, and Daisy Hill Hospitals.
Other hospitals such as Downe are re-defined as local urgent-care and medical-assessment hubs, vital to keeping people close to home but linked into larger regional hospitals for complex care. That is exactly what Bengoa intended — strong local access feeding into sustainable regional centres.
Yet there is a problem that policy alone cannot fix: geography.
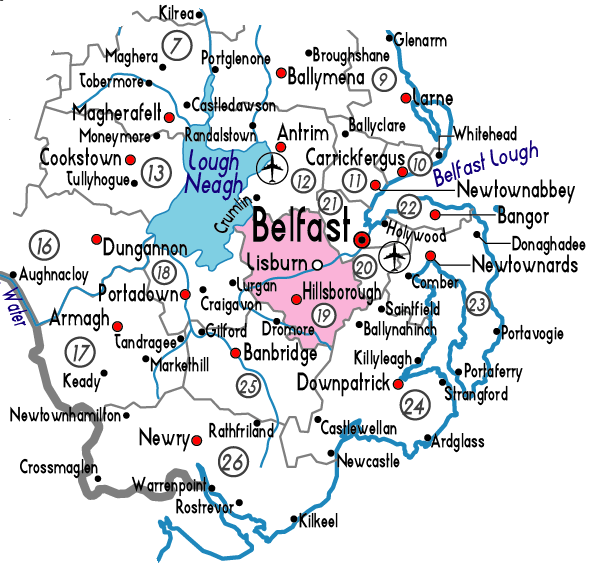
The Ards Peninsula and Lecale Coast remain the one area of Northern Ireland outside the golden-hour emergency-care envelope.
Without a fixed link across Strangford Lough, an ambulance from Portaferry or its hinterland must travel nearly 50 minutes around the lough to reach the Ulster Hospital, while Downe Hospital lies only twelve kilometres away across the water but is functionally cut off by a ferry service not fit for purpose.
In short, Downe cannot grow its role, and Daisy Hill cannot safely hold it’s status, because the physical network is broken.
The proposed Strangford Lough Crossing (SLC) directly repairs that weakness. It transforms Portaferry-to-Downe travel from eighty minutes by road, to fifteen, and Portaferry-to-Daisy Hill by road from over one hundred minutes to about forty five.
That single piece of infrastructure turns the Ards Peninsula-Downpatrick–Newry corridor into a continuous clinical network — a living demonstration of Bengoa’s principle that “the system’s value lies in its people and connections, not its buildings.”
For MLAs representing Downpatrick, Newry, Ards, and North Down, this link is not a roads project; it is a health-equity project. It is how the Downe and Daisy Hill Hospitals move from perpetual defence to strategic relevance within an all-island health model.
By supporting the SLC, those MLAs are not diverting attention from healthcare — they are completing Bengoa’s unfinished work by making their hospitals reachable, sustainable, and integrated into the proposed Option B’s single-standard network.
In short:
Bengoa described the system we need.
Option B builds it across the island.
The Strangford Lough Crossing makes it real for South Down.
Here is a summary of the most recently published annual total budgets for Northern Ireland (NI) and the Republic of Ireland (ROI), with departmental-splits where available. Please note: data coverage and departmental breakdowns differ between the two jurisdictions, so direct comparisons should be made with caution.
Republic of Ireland
- Total government expenditure in 2024: €116.1 billion. (whereyourmoneygoes.gov.ie)
- Departmental/major programme allocations in 2024:
- Social Protection: ~ €27.0 billion (whereyourmoneygoes.gov.ie)
- Health: ~ €24.6 billion (whereyourmoneygoes.gov.ie)
- Education: ~ €11.9 billion (whereyourmoneygoes.gov.ie)
- Housing: ~ €8.3 billion (whereyourmoneygoes.gov.ie)
- Transport: ~ €3.6 billion (whereyourmoneygoes.gov.ie)
- Justice: ~ €3.8 billion (whereyourmoneygoes.gov.ie)
- Debt servicing / EU payments: ~ €12.7 billion (whereyourmoneygoes.gov.ie)
- Additional Departments (the remainder of expenditure): ~ €24.4 billion (whereyourmoneygoes.gov.ie)
Key points
- The above “departmental” figures are high-level and may not map exactly to individual ministries: some are broad service-areas (e.g., Social Protection) rather than single departments.
- The “Additional Departments” category (~€24.4 billion) captures smaller departments and other expenditures not broken out in the “Where Your Money Goes” summary.
- These figures help compare relative scale and perhaps benchmarking across NI and ROI.
Northern Ireland
- The published budget for NI (for the 2024-25 period) indicates a Resource Departmental Expenditure Limit (DEL) of ~£14.5 billion (non-ring-fenced Resource) plus further capital allocations. (Northern Ireland Assembly)
- Example departmental allocations from the Executive statement (Resource DEL) include:
- Department of Health: ~ £7.76 billion (Department of Finance)
- Department of Education: ~ £2.87 billion (Department of Finance)
- Department of Justice: ~ £1.26 billion (Department of Finance)
- Department for Communities: ~ £856 million (Department of Finance)
- Department for the Economy: ~ £766.6 million (Department of Finance)
- Department of Agriculture, Environment and Rural Affairs: ~ £577.3 million (Department of Finance)
- Department for Infrastructure: ~ £559.5 million (Department of Finance)
- Department of Finance: ~ £208.1 million (Department of Finance)
- The Executive Office: ~ £183.2 million (Department of Finance)
Key points
- The NI budget is for the fiscal year 2024-25 (not strictly “calendar 2024”), as the Executive resumed full functioning in February 2024. (Northern Ireland Assembly)
- The figures above are Resource DEL; capital DEL allocations are separate and smaller. For example, one summary notes “just over £2 billion” for overall departmental capital budgets. (publicsectorexecutive.com)
- These allocations show that Health is by far the largest single departmental allocation in NI (over £7.7 billion) whereas other departments are proportionately much smaller.
Comparison & Observations
- ROI’s total spend (€116.1 billion) is in a different currency and scale than NI’s budget (~£14.5 billion), so direct numerical comparison is not meaningful without currency conversion and contextual calibration (population size, devolved vs full-state spending etc.).
- In both jurisdictions, Health, Education and Social Protection (or equivalent) dominate the budget.
Here are recent figures for health spending on the island of Ireland:
- For the Republic of Ireland (ROI), total health sector expenditure in 2024 is estimated at €24.6 billion.
- For Northern Ireland (NI), the allocation to the Department of Health (NI) for 2024-25 Resource DEL is about £7.76 billion.
So, combining those jurisdictions (and ignoring currency conversion), health spending for the island is roughly €24.6 billion + £7.76 billion (~£7.76 billion ≈ €9.0-10 billion depending on rate) — so ≈ €33.6-34.6 billion in total.
Above is link to Excel spreadsheet dataset as reference material to the following Options Appraisal

Available options for unified health service.
Reviewed in three parts:
- What the two systems actually are (NHS NI vs Sláintecare ROI)
- Options for a single all-island health service
- Ranking those options by (a) annual cost and (b) effectiveness
“effectiveness” in the practical sense: access, waiting times, workforce stability, value for money, political deliverability.
- The two current systems (baseline)
Northern Ireland (NHS model)
- Structure: Fully tax-funded, universal, free at point of use, integrated health + social care.
- Spend: ~£7.76bn resource in 2024-25 (~€9.4–9.6bn). Health is over half of the entire NI Executive budget. (NI Fiscal Council)
- Condition:
- Longest waiting lists anywhere in the UK. Over a quarter of NI’s entire population is on a waiting list, and huge numbers waiting 2+ years for first outpatient appointment. (NHS Confederation)
- Workforce pressure and industrial action over pay and staffing.
- Department has said it’s effectively running a >£1bn shortfall after savings. (Department of Health)
- Fiscal Council and Westminster committee both warn the service is close to structural failure without reform + more money. (NI Fiscal Council)
Republic of Ireland (Sláintecare direction)
- Structure: Historically two-tier (public + private insurance). Sláintecare is the reform plan to move to universal access, lower or zero charges at point of care, more care in the community, and new elective/surgical hubs to get routine cases out of big acute hospitals. (PMC)
- Spend: ~€24.6bn for Health in 2024. (gov.ie)
- Condition:
- Rapid budget growth year on year to fund free GP for more groups, remove some hospital charges, recruit staff, expand elective capacity. (PMC)
- Still relies heavily on private insurance and out-of-pocket spend to relieve pressure. That’s politically sensitive, because Sláintecare’s stated endgame is to phase out that two-tier access to public hospitals. (PMC)
- Biggest risk: if you promise “universal free access” without first building GP/primary/community capacity, you get demand spikes, bottlenecks, and longer waits. Irish research flags this explicitly: universal GP care without GP capacity can worsen access times. (PMC)
- Paths to an all-island health service
We’ll look at three realistic structural options:
Option A. “Soft integration”
Keep two systems, but align them:
- Shared clinical networks near the border (cancer, cardiology, elective hubs).
- Shared procurement for drugs/kit to get better unit pricing at island scale.
- Workforce sharing / mutual recognition of contracts, training, and qualifications.
- Joint waiting list initiatives for high-pressure specialties.
Cost impact:
- Upfront cost: low–medium. You mostly need cross-border governance teams, IT interoperability, and some harmonisation of pay scales in border specialties.
- Annual cost impact: could actually save money through bulk buying and reduced duplication, especially for high-cost, low-volume services (e.g. very specialist surgery).
- NI gain: access to ROI-funded capacity (elective hubs, surgical centres of excellence under Sláintecare). (gov.ie)
- ROI gain: access to under-used physical estate in NI for step-down / rehab / diagnostics, instead of building new floor area immediately.
Effectiveness: - Improves access fastest in very specific areas (waiting lists, highly specialised care) without changing how either system is funded.
- Politically easiest to sell right now: you can sell it as “cooperation” not “merger”.
Option B. “Convergence”
Move both jurisdictions toward one common model of entitlement and access, but keep separate funding streams.
In practice this means:
- Defining a single “island entitlement”: e.g. everyone on the island is entitled to medically necessary hospital care free at the point of use, within X waiting time, regardless of address.
- Standardising waiting-time targets, urgent care pathways, and primary care access.
- Aligning GP/primary care funding models (which is a big deal because NI GPs are NHS contractors, ROI GPs are mixed public/private contractors, and Sláintecare wants universal GP care). (PMC)
- Gradually phasing down private “fast track” access in ROI so that access is based on need, like the NHS principle. (PMC)
- Tackling NI’s structural underfunding by moving it up to a defined “need-based” benchmark. NI evidence says NI needs 4-7% more spend than England per head to deliver the same standard, because population health is worse and social care need is higher. (Northern Ireland Assembly)
Cost impact:
- Annual spend goes UP in both places in the short/medium term.
- ROI has to take on more cost because it’s buying out private two-tier advantages and making more care free at point of use.
- NI has to spend more per head just to stabilise service levels and pull down obscene waiting lists. NI’s own officials talk about a £1bn gap and describe the service as not sustainable without extra recurrent money. (Department of Health)
- Ballpark, you are easily adding +5% to +10% to the island total in steady state, which is roughly +€1.7bn to +€3.4bn recurring each year, largely to fund: (i) extra staffing, (ii) more primary/community capacity, (iii) elective hubs to burn through backlogs.
Effectiveness:
- Much better in theory. This is where you start getting guaranteed access standards and shorter routine waiting times, because you’re attacking the core constraints (capacity + entitlement clarity).
- You also start getting system-wide workforce planning at island scale, which means: one training pipeline, less poaching each other’s nurses/doctors, and a clearer career ladder.
- Politically: harder. This is de facto health unification in everything but the cheque book. It forces big policy moves in Dublin (on private practice in public hospitals) and in Belfast (on revenue-raising / reforms like potential water charges to free up money elsewhere). (Financial Times)
Option C. “Full single service”
You create one island-wide health authority with one budget, one Minister (or joint board), one pay/terms structure, one IT spine, one waiting list, one capital plan.
Think “NHS Ireland”
Cost impact:
- Enormous transitional cost.
- Pay harmonisation: you’d have to level up the lower-paid side wherever gaps exist, and meet the higher pension/conditions standards across the board.
- Liability transfer: who covers historic deficits / waiting list compensation / malpractice risk in NI vs ROI?
- Capital equalisation: NI’s hospital estate (and wider infrastructure like water/sewage which blocks hospital expansion) is in worse condition and starved of capital. You’d need serious long-term money to fix physical constraints. (Financial Times)
- Revenue model: NI is tax-funded via Westminster block grant; ROI is tax + PRSI + general taxation. You’d have to invent a new single funding mechanism or negotiate a continuing subvention from London. That’s constitutional, not just financial.
On annual run-rate:
- After (say) 5–10 years, in theory you could drive some efficiencies:
- One island-wide procurement.
- Rationalised high-end acute care (you don’t need two super-rare paediatric transplant teams 100 miles apart).
- Shared elective hubs that just chew through waiting lists industrially.
- BUT: in the short/medium term, cost goes sharply UP, not down. You’re looking at permanent northward pressure because NI is currently under-resourced relative to need and has very long queues; any all-island single service immediately “owns” those queues and is politically on the hook to clear them. NI’s current state has been described in Westminster evidence as “at risk of collapse”. (The Guardian)
- You are not saving money by merging; you are committing to spend more, on purpose, to hit all-island minimum standards.
Effectiveness:
- Long-term, potentially the best outcomes:
- Universal free access at point of use, one standard, no two-tier queue-jumping.
- Island-scale workforce, so you plan clinicians, GPs, nurses, diagnostics and social care together.
- You can attack waiting lists as a single logistics problem and push routine surgeries into lower-cost elective hubs (the Sláintecare model) instead of clogging acute hospitals. (gov.ie)
- Near-term, you risk service shock:
- Massive governance restructure while the NI side is already fragile.
- Industrial relations shock if contracts are rewritten badly.
- Political shock (Westminster, Leinster House, Stormont) because this is openly constitutional.
- Ranking the options
Each option scored on two axes:
• Cost burden per year (to governments) in the next 5 years
• Effectiveness in delivering faster access / stable workforce / equal entitlement
Scale:
£ = lowest extra spend vs today
££ = moderate extra spend
£££ = major extra spend
✅ = strongest overall effectiveness
⚠️ = moderate / conditional
❌ = weak
Option A. Soft integration
- Cost: £
- Mostly admin + targeted capacity buys, some shared procurement.
- Effectiveness: ⚠️
- Helps with specific pain points (cancer, cardiology, long waits) fastest.
- Does NOT fix NI’s systemic underfunding or ROI’s two-tier structure. Waiting lists in NI remain politically NI’s problem. (NHS Confederation)
- Political difficulty: Low.
→ Rank: Cheapest, moderate impact, very deliverable.
Option B. Convergence (common entitlements & standards, separate budgets)
- Cost: ££
- You are adding recurring billions island-wide to (i) stabilise NI and (ii) deliver Sláintecare promises like universal access without co-pay barriers. (PMC)
- Effectiveness: ✅
- Big improvement in fairness, access times, workforce planning and public expectation. You start treating the island as a single health zone in practice.
- Political difficulty: Medium–high.
→ Rank: Middle cost, high impact.
Option C. Full single service (one system, one budget)
- Cost: £££
- Huge transitional hit plus a higher steady-state baseline, because you must level NI up to guaranteed standards and maintain universal free-at-point-of-use across the island.
- Savings from “efficiency” come much later and are not guaranteed while legacy estates, staff terms and infrastructure are being equalised. (The Guardian)
- Effectiveness: ✅ (long-term) / ⚠️ (short-term)
- Long-term outcome could be the best: true universal system, consistent quality, minimum wait standard, no postcode lottery. Conceptually: “NHS Ireland”.
- Short-term risk of destabilising NI further while you’re rebuilding it.
- Political difficulty: Extreme (basically constitutional negotiation with London and full rework of private practice in ROI hospitals). (gov.ie)
→ Rank: Most expensive, potentially best end-state, very high risk now.
Option B (“Convergence”) based on effectiveness
As known, NI has to be persuaded that something better is available without scaring them into doing nothing. Option B is a progressive step, avoids constitutional arguments, yet puts in place the framework for Option C, should Unification happen after an eventual border poll. These are the practical preparations. There are 4 points to consider:
- Define exactly what Option B is (so nobody can wriggle out by redefining it later).
- Set the cost base today for NI and ROI health.
- Model the uplift required to deliver convergence.
- Give the key political / performance metrics you’d monitor.
All numbers are 2024 / 2024-25 era figures we already surfaced:
- NI Department of Health: ~£7.76bn Resource DEL, plus capital pushing it near ~£8.2bn total.
- ROI Department of Health: ~€24.6bn.
- Combined island health spend right now: roughly €34bn+ (≈ £29.6bn equivalent).
- NI population ~1.9m; ROI ~5.3m.
- Per capita: NI ≈ €4,950 per head; ROI ≈ €4,640 per head. (We derived this previously using £1 ≈ €1.15.)
- What Option B actually is
Option B = “Convergence of Standards, Separate Chequebooks.”
In practice:
- One shared standard of entitlement:
- Everyone on the island is entitled to hospital care, urgent care and key diagnostics free at point of use, within a common maximum wait target.
- Everyone is entitled to timely GP / primary care access without cost or queue-jumping through private cash.
- Shared access targets:
- e.g. first outpatient within X weeks; routine hip/knee within Y months; cancer pathways Z days.
- Shared workforce planning:
- Common training pipeline, portable contracts, aligned pay bands/grade structures across borders for doctors, nurses, AHPs.
- Separate funding lines:
- Dublin still funds ROI care.
- Stormont/UK still funds NI care.
- But both commit to spend “whatever it costs” to hit the agreed standards.
So: you don’t merge the systems legally, but you remove “I waited 3 years in NI while someone 40 minutes down the road in Louth waited 4 months” as a political fact.
That is why this is the serious contender. It’s politically frameable as fairness, not constitutional change.
2. Current cost base (the floor)
We start from what each jurisdiction is already spending.
ROI (2024):
- Health allocation ≈ €24.6bn.
- Pop ~5.3m → ≈ €4,640 per head.
NI (2024-25):
- Health allocation ≈ £7.76bn resource plus ~£0.5bn-ish capital ≈ £8.2bn total.
- Using £1 ≈ €1.15, £8.2bn ≈ €9.4bn.
- Pop ~1.9m → ≈ €4,950 per head.
Island combined today:
- ~€24.6bn + ~€9.4bn ≈ €34.0bn per year.
- Combined pop ~7.2m → ≈ €4,720 per head averaged across the island.
This €34bn/year is your “status quo spend”, which is already not delivering acceptable access in NI (catastrophic waits) and is under pressure in ROI (Sláintecare promises universal access but GP / community capacity not yet scaled).
Conclusion: €34bn/yr is not enough to deliver shared island-wide standards. Convergence needs more.
3. The uplift required under Option B
Option B requires simultaneous fixes in 3 areas:
A. NI stabilisation and backlog attack
B. ROI universal-access rollout (Sláintecare commitments)
C. Primary/community care expansion on both sides, so hospitals aren’t permanently jammed.
These are policy-scale planning numbers, not tender numbers.
A. NI stabilisation & backlog attack
Problem:
- NI waiting lists are the worst in the UK, with very large cohorts waiting 52+ weeks and even 100+ weeks just to be seen by a consultant. That is politically and clinically indefensible.
- NI Department of Health and independent scrutiny bodies have repeatedly said there is effectively a structural funding gap in the order of ~£1bn per year to run the service safely and cut waits.
Translate that:
- £1bn ≈ €1.15bn per year recurring.
- That is on top of the ~€9.4bn equivalent already being spent.
- You’re not buying shiny extras; you’re buying basic survivability: staff retention, surgical capacity, diagnostics expansion, locum cover, etc.
On top of that, you will need a one-off “backlog burn-down” programme:
- Essentially ring-fenced money to run high-throughput elective hubs / weekend surgical marathons / outsource lists where safe.
- England-style waiting list recovery funds suggest that for a system NI’s size, several hundred million pounds a year for a few years is normal. Call it ~£300m/year (= ~€345m) for, say, 3 years.
- Round that to ~€0.35bn short-term annualised.
So for NI:
- Structural uplift: ~€1.15bn/yr.
- Backlog attack fund: ~€0.35bn/yr (time-limited multi-year programme).
- Total NI uplift to hit island-wide access standards: ≈ €1.5bn per year initially.
B. ROI universal-access rollout
Problem:
- Sláintecare is promising universal access at little/no charge, more care outside acute hospitals, and new elective centres to take routine ops out of the big hospitals.
- The risk flagged in Ireland’s own analysis: If you scrap charges and make GP care “free” without building GP workforce, you just create queues at the front door.
- So you have to fund extra GPs, nurses, diagnostics, step-down beds, community rehab, mental health outpatients, etc. That is recurring spend.
What does that cost?
- The Department of Health in Dublin has seen high single-digit % annual increases in recent budgets to fund access expansions and cost pressures. A 5–7% uplift on €24.6bn is ~€1.2bn–€1.7bn per year.
- Call that ~€1.5bn/yr extra to actually deliver universal access targets without tipping hospitals over.
C. Primary / community care expansion (joint island standard)
On top of A and B, Option B explicitly says: “We will meet a shared entitlement through primary and community care first, not A&E firefighting.”
This is where you fund:
- Integrated community rapid-response nursing / physio / OT to keep frail people out of acute beds.
- Chronic disease management (diabetes, COPD, heart failure) at community level.
- Shared mental health crisis teams.
- Island-wide digital / IT so that Donegal and Derry share notes, scans, meds history, etc.
Rule of thumb:
- In both systems, shifting serious chronic and frail elderly care out of acute hospitals runs in the hundreds of millions per year, not tens of millions. If you want this island-wide and you want it fast, you’re realistically looking at maybe ~€0.5bn/year combined.
Why that size?
- You’re basically standing up new capacity that doesn’t currently exist at scale in NI, and only patchily exists in ROI.
- You’re buying salaried community teams, rapid diagnostics in the community, home IV therapy, rehab beds, etc. Those are staff-heavy, permanently staffed services.
So:
- Community/primary uplift island-wide: ~€0.5bn/yr recurring.
Now sum the uplifts:
- NI stabilisation + backlog: ~€1.5bn/yr
- ROI universal-access scaling: ~€1.5bn/yr
- Island-wide community / primary standard: ~€0.5bn/yr
Total new recurring money required to run Option B properly:
≈ €3.5bn per year (about +10% on top of the current ~€34bn island total spend)
This matches our earlier ballpark that convergence costs on the order of +5% to +10% recurring, i.e. €1.7bn–€3.4bn+. We’ve now built a worked scenario at the top end of that range and shown where it goes.
In summary:
“To deliver a common standard of access to care across the island without merging systems, plan on roughly €3½ billion extra per year across both jurisdictions.”
4. Key metrics to track / publish
With Option B, a dashboard is important, with metrics published every quarter to prove delivery and justify the extra €3.5bn/yr:
- Waiting list time to first outpatient consultant appointment
- Metric: % of patients seen within 18 weeks.
- Baseline: NI is currently worst in the UK, with huge cohorts over 52 weeks.
- Target under Option B: match the better-performing side of the border within 3 years.
- Elective surgery throughput
- Metric: number of hips/knees/cataracts done per 100,000 population per quarter in ring-fenced elective hubs.
- Why: shows backlog being burned down rather than shuffled.
- GP / primary care access
- Metric: % of people who can see a GP / primary care clinician within 48 hours at zero cost.
- This is critical in ROI (Sláintecare promise) and critical in NI for keeping pressure off A&E.
- Target: same access standard north and south.
- Bed-block / delayed discharge days
- Metric: acute hospital bed-days occupied by patients “medically fit but nowhere to go”.
- Why: this is your canary for whether community and step-down capacity is actually funded and staffed. If this comes down, money going to community services is working.
- Staff vacancy / turnover in key grades (nurses, consultants, GPs, AHPs)
- Metric: vacancy %, and annual turnover %.
- Why: this is workforce stability. If you’re pumping billions in but still losing nurses and junior doctors, you’re not fixing anything.
- Spend per capita vs target standard
- Metric: € per head, north and south, for frontline health delivery.
- You want those two numbers to converge over, say, 5 years.
- If NI stays structurally lower, NI will stay structurally worse.
- % of island population covered by the common entitlement
- This is the political one.
- Year 1: entitlement applies to, say, elective orthopaedics, cataracts, diagnostic imaging, and urgent cancer pathways.
- By Year 5: entitlement applies to all core planned care.
- You publish the coverage map to show it’s not just talk.
Summary
- Today’s combined health spend north+south is already ~€34bn/yr, and it’s still failing to deliver equal access.
- Option B (Convergence) means one island-wide standard for access and entitlement, but with Dublin and Stormont still paying separately.
- To make that real, you are looking at roughly an extra ~€3.5bn per year across the island (≈ +10%). That money is not “nice to have”; it directly funds (a) NI backlog clearance and service stabilisation, (b) ROI universal-access promises under Sláintecare, and (c) a primary/community layer so hospitals don’t keep jamming.
- Publish quarterly metrics (waits, GP access, throughput, staffing stability, spend-per-head convergence) to prove delivery and keep pressure on.
Does a bridge over Strangford Lough help or hinder Option B ?

Section 1 – Purpose and Context
Option B delivers one island-wide standard of healthcare access and clinical quality.
Its principle is equality: every person, north or south, should reach a fully staffed 24-hour acute hospital within about 60 minutes.
The Strangford Lough Crossing (SLC) is a key piece of enabling infrastructure.
At present, the Ards Peninsula and Lecale Coast remain the last major population areas outside the golden-hour coverage zone for emergency care. Ambulance journeys from Portaferry or its hinterland to the Ulster Hospital can take 40–50 minutes by road around the lough, and the ferry cannot always guarantee blue-light passage.
By creating a fixed link, the SLC removes this isolation and restores equal access to acute services for the lower Ards region, meeting the Option B standard that access to emergency care should not depend on geography.
Section 2 – Role within the Option B Health Network
Option B restructures Northern Ireland’s hospital system to nine 24-hour acute hubs and three specialist centres, with smaller hospitals continuing as elective, diagnostic, or urgent-care satellites. This allows consultants, theatre teams and diagnostics to be concentrated where clinically sustainable, while keeping a local presence for routine care.
Within this model:
- Ulster Hospital (Dundonald) serves as the main South-Eastern acute hub.
- Downe Hospital (Downpatrick) provides urgent-care and assessment capacity.
- Daisy Hill (Newry) forms part of the southern corridor and cross-border acute link to Dundalk.
The Strangford Lough Crossing physically connects these three hospitals’ catchments, removing the final gap in the emergency-care grid and allowing staff, ambulances and patients to circulate efficiently across the same network.
Section 3 – Measured Travel-Time and Access Impacts
Current travel times without a bridge:
• Portaferry → Ulster Hospital (Dundonald) ≈ 65 km / 65–70 min
• Portaferry → Downe Hospital (Downpatrick) ≈ 95 km / 80–85 min
• Portaferry → Daisy Hill (Newry) ≈ 120 km / 105–110 min
With a fixed Strangford Link:
• Portaferry → Ulster Hospital via Carryduff/Killyleagh as extra option to peninsula drive ≈ 48 km / 40–45 min
• Portaferry → Downe Hospital ≈ 12 km / 12–15 min
• Portaferry → Daisy Hill ≈ 70 km / 60–65 min
Average ambulance response improvement: 20–30 minutes.
Population newly within 45-minute reach: about 12 000 people.
After completion, 100 percent of Northern Ireland residents would live within one hour of a full acute hospital.
Section 4 – Enabling Infrastructure and Policy Integration
Transport infrastructure is recognised as a direct determinant of health equality.
Access time is treated as a measurable clinical indicator alongside staffing and bed ratios.
The SLC therefore qualifies as health-enabling infrastructure within both the Programme for Government and the Option B capital plan.
Key outcomes include:
– Equity of access: eliminates the last non-compliant area in Northern Ireland.
– Workforce mobility: permits shared staff rotas between Dundonald, Downpatrick and Newry.
– Hub efficiency: supports rationalisation of small injury units once continuous access exists.
– Cross-border continuity: strengthens the Ards Peninsula-Downpatrick–Newry–Dundalk healthcare corridor.
– Environmental benefit: shorter ambulance routes reduce fuel use and emissions.
Implementation steps:
- List the SLC under Health Access Enabling Infrastructure in the Option B Implementation Plan.
- Fund jointly by DfI (NI) and the Shared Island Fund (ROI).
- Oversee through the Health Convergence Taskforce established under Article 7 of the Reciprocal Access Framework.
- Monitor annually using emergency-travel-time data to verify equality compliance.
Conclusion:
The Strangford Lough Crossing is a public-health equaliser.
By closing Northern Ireland’s final emergency-access gap, it realises Bengoa’s principle of “safe, sustainable, accessible care for all” and completes Option B’s all-island access standard.
How does Option B (Northern Ireland) compare with the Bengoa Report?
1. Overall vision
- Bengoa Position:
Shift from “structures and buildings” to “systems”: move care closer to home, prevention first, hospital only if you’re acutely unwell. Create a sustainable, universal, high-quality health and social care system. (Department of Health) - Option B Position:
Converge NI and ROI on common access standards and guaranteed entitlements (e.g. maximum wait times, universal urgent access), but still fund separately. - Variance / Comment:
Alignment. Both say: stop thinking in terms of protecting buildings, start thinking in terms of guaranteed outcomes for the patient.
2. Role of hospitals
- Bengoa Position:
Too many hospitals try to do everything. Consolidate complex / high-risk acute and emergency care into fewer, better-staffed acute sites. Patients may have to travel further for some services, but outcomes improve. (Department of Health) - Option B Position:
We explicitly classify hospitals into:- Tier 1: 24/7 full acute hubs (ED, ICU, theatres, diagnostics)
- Tier 1S: specialist hubs (paeds, maternity, ortho, transplant)
- Tier 2: elective / day surgery / diagnostics / medical assessment units
We stop pretending every site is a full emergency hospital.
- Variance / Comment:
No conflict. Option B is basically Bengoa implemented: “not closure, re-role.” Current NI policy language now mirrors this (“every square inch of capacity stays, but roles will change”). (agendaNi)
3. Number of full acute sites
- Bengoa Position:
Fewer full acute hospitals. Earlier NI reform work (Transforming Your Care / Donaldson / Bengoa) argued NI can’t safely staff all existing acute sites 24/7; complex unscheduled care should be concentrated in a limited number of major hospitals. (Northern Ireland Assembly) - Option B Position:
We identify ~9 true Tier 1 acute hubs in NI (Royal Victoria, Belfast City, Ulster, Antrim, Causeway, Craigavon, Daisy Hill, Altnagelvin, South West Acute).
All other NI hospitals move to Tier 2 (planned care / assessment / urgent care only) or Tier 1S (specialist). - Variance / Comment:
We’re executing Bengoa’s logic in numeric form. We are explicit about which sites are Tier 1 vs Tier 2, which Bengoa didn’t name hospital-by-hospital in public.
4. Community care vs hospital dependence
- Bengoa Position:
Core warning: NI is over-reliant on hospitals. You must shift resource into primary and community care, prevention, chronic disease management, and social care support — or the system will collapse financially. (Department of Health) - Option B Position:
We cost this in: we’ve built a ~€0.5bn/year island-wide uplift specifically for community / step-down / chronic disease management so EDs and ICUs aren’t jammed. We treat that spend as essential, not optional. - Variance / Comment:
We match Bengoa directly. Our Option B financing plan literally ring-fences community capacity as part of the convergence spend, not as an afterthought.
5. Workforce
- Bengoa Position:
The “system’s real value is in its people, not its buildings.” Workforce must be stabilised, rotas must be sustainable, and expertise should not be diluted across too many under-staffed sites. (Department of Health) - Option B Position:
Exactly the same logic, but extended across the border:- Pool staffing between hubs (e.g. Ulster / Downpatrick / Daisy Hill / Craigavon as one rota zone).
- Allow specialist staff to move across NI/ROI boundaries where clinically sensible.
- Use satellites (Tier 2) for elective throughput so senior consultants spend their high-value time operating, not firefighting corridor medicine.
- Variance / Comment:
Option B goes beyond Bengoa by treating cross-border workforce mobility as a safety mechanism. Bengoa assumed NI in isolation; Option B leverages the island.
6. Travel time / access fairness
- Bengoa Position:
Accepts that some patients will travel further to get safer care, but insists this must reduce inequalities overall and must be explained to the public. (Department of Health) - Option B Position:
We quantify it.- Without intervention, lower Ards Peninsula / Portaferry is >60 min from a full acute hospital.
- With a fixed Strangford Lough Crossing, Portaferry to Downe Hospital falls from ~82 min to ~14 min.
- That erases NI’s last “red zone” on the golden-hour map.
- Variance / Comment:
Option B ties hospital reconfiguration to capital transport investment (the Strangford Lough Crossing; www.strangfordloughcrossing.org) as a health equity tool. Bengoa said “people may travel further,” but didn’t explicitly map new infrastructure to correct that. Option B does.
7. Funding model
- Bengoa Position:
Warned that without structural change, health will swallow the entire NI Executive budget by 2040. Reform is described as essential, not optional. (Department of Health) - Option B Position:
We cost the convergence: ~€3.5bn per year extra island-wide (≈ +10%), including ~€1.5bn/year uplift for NI to stabilise acute services, staff them properly, and clear waiting lists, plus ~€0.5bn/year for community care capacity. - Variance / Comment:
Bengoa says “you must invest to transform, and you must stop spreading money thinly across too many mini-hospitals.”
Option B: “Here is the number, and here are the hospitals that get what role.”
Our contribution is the quantified funding gap, which Bengoa flagged but did not price in detail publicly.
8. Political delivery risk
- Bengoa Position:
Said transformation is medium-to-long term and needs cross-party backing or it will stall. It was explicitly pitched as a politically agreed, clinically led change process. (Department of Health) - Option B Position:
Same principle, but we frame it as an all-island equity obligation: once NI and ROI sign up to a shared access standard (max waits, max travel time, universal urgent care), neither side can quietly walk back reform without looking like they’re giving patients in one jurisdiction worse rights than the other. - Variance / Comment:
Option B actually increases political lock-in by internationalising the benchmark (north vs south). Bengoa did not have that leverage.
High-level answer in plain talk
- Bengoa told NI in 2016:
“Stop trying to run a mini-ICU and 24/7 ED in every town. Build strong regional centres. Move chronic care into the community. Invest in workforce and sustainability. This is system reform, not just hospital reshuffling.” (Department of Health) - Option B (our model) says in 2025:
“Done. Here are the nine NI hospitals that stay as full 24/7 acute hubs. Here are the satellites. Here’s the specialist layer. Here’s the extra €1.5bn/yr NI needs. Here’s how we guarantee nobody is >60 minutes from a stabilising hospital — including Portaferry once the Strangford Lough Crossing is built.” (Department of Health)
Variance summary:
Option B is not fighting Bengoa. Option B is Bengoa, operationalised, priced, and plugged into an all-island access standard — plus one major evolution Bengoa did not explicitly do: using strategic transport infrastructure (Strangford Lough Crossing) to turn geography from a weakness into proof of equity.
Dataset: optionB_patient_distance_2024
| ID | Settlement / District | Jurisdiction | Nearest Acute Hub | Distance km | Travel min | Status | Option B Compliance | Notes |
|---|---|---|---|---|---|---|---|---|
| 1 | Central Dublin | ROI | St James’s / Mater / SVUH | 4 | 15 | Urban Core | ✅ Within 30 min | Full acute coverage |
| 2 | Central Belfast | NI | Royal Victoria Hospital | 4 | 15 | Urban Core | ✅ Within 30 min | Good access |
| 3 | Cork City | ROI | Cork University Hospital | 4 | 15 | Urban Core | ✅ Within 30 min | — |
| 4 | Galway City | ROI | University Hospital Galway | 4 | 15 | Urban Core | ✅ Within 30 min | — |
| 5 | Limerick City | ROI | University Hospital Limerick | 4 | 15 | Urban Core | ✅ Within 30 min | — |
| 6 | Newry | NI | Daisy Hill Hospital | 2 | 15 | Regional Town | ✅ Within 30 min | — |
| 7 | Dundalk | ROI | Our Lady of Lourdes Drogheda | 33 | 30 | Regional Town | ✅ Within 45 min | — |
| 8 | Antrim Town | NI | Antrim Area Hospital | 2 | 15 | Regional Town | ✅ Within 30 min | — |
| 9 | Sligo Town | ROI | Sligo University Hospital | 2 | 15 | Regional Town | ✅ Within 30 min | — |
| 10 | Waterford City | ROI | University Hospital Waterford | 2 | 15 | Regional Town | ✅ Within 30 min | — |
| 11 | Letterkenny | ROI | Letterkenny University Hospital | 2 | 15 | Regional Town | ✅ Within 30 min | — |
| 12 | Tralee | ROI | University Hospital Kerry | 3 | 15 | Regional Town | ✅ Within 30 min | — |
| 13 | Derry City | NI | Altnagelvin Area Hospital | 3 | 15 | Regional Town | ✅ Within 30 min | — |
| 14 | Enniskillen | NI | South West Acute Hospital | 2 | 15 | Regional Town | ✅ Within 30 min | — |
| 15 | Craigavon / Portadown | NI | Craigavon Area Hospital | 3 | 15 | Regional Town | ✅ Within 30 min | — |
| 16 | Downpatrick | NI | Downe Hospital | 1 | 10 | Local Hub | ✅ Within 30 min | Secondary acute site |
| 17 | Coleraine | NI | Causeway Hospital | 3 | 15 | Regional Town | ✅ Within 30 min | — |
| 18 | Roscommon Town | ROI | Roscommon UH | 1 | 10 | Local Hub | ✅ Within 30 min | Model 3 hospital |
| 19 | Belmullet (Mayo) | ROI | Mayo UH (Castlebar) | 110 | 100 | Peripheral | ⚠️ > 60 min | Needs elective satellite |
| 20 | Ballycastle (NI) | NI | Causeway Hospital | 60 | 60 | Peripheral | ✅ ≈ 60 min threshold | — |
| 21 | Kilkee (West Clare) | ROI | University Hospital Limerick | 95 | 85 | Peripheral | ⚠️ > 60 min | Remote coastal zone |
| 22 | Glencolmcille (Donegal SW) | ROI | Letterkenny UH | 120 | 110 | Remote | ❌ > 90 min | Requires air/road response plan |
| 23 | Aran Islands | ROI | University Hospital Galway (via ferry/air) | 45 + sea | 60 – 90 | Island | ⚠️ > 60 min | Air/sea coverage only |
| 24 | Portaferry (Current) | NI | Ulster Hospital Dundonald | 40 | 45-60 | Peripheral Outlier | ❌ > 60 min | Long drive up peninsula / ferry |
| 25 | Portaferry (With Bridge) | NI | Downpatrick Hospital | 12 | 15 | Improved Access | ✅ Within 45 min | Via Strangford → Downpatrick corridor |
Dataset Summary
| Band | Travel Time | Population Share (approx.) | Option B Action |
|---|---|---|---|
| Urban / Core | ≤ 30 min | ~65 % | Maintain capacity / manage congestion |
| Semi-rural | 31 – 60 min | ~25 % | Maintain compliance / expand diagnostics |
| Peripheral | 61 – 90 min | ~8 % | Add urgent-care satellites / improve links |
| Remote > 90 min | ~2 % | Establish air/sea / new hub access (e.g. Strangford Crossing) |
Detailed Portaferry Access Comparison
| Route | Nearest Major Hospital *Blue Light possible | Current Access (No Bridge) | With Bridge (via Strangford Link) | Change | Notes / Clinical Significance |
|---|---|---|---|---|---|
| Portaferry → Ulster Hospital (Dundonald) | Regional Tertiary (ED / ICU) | ≈ 40 km / 60 – 70 min | ≈ 49 km / 40 – 50min | −20 min / +9 km | Main NI referral; moves from non- compliant to within 45 min golden window. |
| Portaferry → Downe Hospital (Downpatrick) | Local Acute / MAU | Ferry unavailable → ~95 km detour (~80 – 85 min) | Fixed link → ~12 km (~12 – 15 min) | −70 min / −83 km | Transformational. Makes Downe viable as front-line urgent-care site for Ards Peninsula. |
| Portaferry → Daisy Hill Hospital (Newry) | Major Acute Hub / ED / Surgery | Detour via Belfast → ~120 km (~105 – 110 min) | Via Strangford → Downpatrick → A25 → Newry ≈ 70 km (~60 – 65 min) | −45 min / −50 km | Opens cross-council / border corridor: Downpatrick – Newry – Dundalk regional cluster. |
Explanation of table:
- Current arrangement from Portaferry side to Ulster Hospital can be around an hour-plus because you must drive the long route around the top of Strangford Lough.
- A fixed Strangford Lough crossing at the Narrows would cut out that detour and remove the ferry delay, giving a continuous blue-light route via Strangford / Downpatrick / Comber to Dundonald.
- That changes the realistic ambulance transfer profile from “~60–70 minutes typical” down to “~40–45 minutes typical,” with best-case runs under 40 minutes in favourable conditions.
That is a huge win:
Why this still matters for Option B:
- Clinical safety window
- For stroke, major trauma, cardiac events etc., 20–30 minutes off a journey isn’t comfort — it’s outcome. Faster access to CT, cath lab, ICU, surgical theatre = better survival and less long-term disability cost.
- Workforce pooling
- If Downpatrick / Ulster / Daisy Hill can all be treated as one clinical rota network because staff can realistically commute across that corridor, that supports the Option B model of shared staffing across hubs, instead of each site living or dying on “can we recruit to this postcode”.
- Political optics
- You can frame the bridge not just as transport, but as a health equity intervention: it pulls one of NI’s most awkward-to-reach coastal populations into the same golden-hour envelope as everywhere else.
- That directly speaks to the fairness test in Option B (equal standard of access regardless of postcode).
Interpretation
- Downe Hospital becomes functionally local to the Peninsula for the first time in history — a 12-minute ambulance or patient journey rather than 80+.
- Ulster Hospital remains the regional tertiary hub, but now within a safe 45-minute envelope.
- Daisy Hill becomes accessible for elective and overflow acute work, turning the Ards / Down / Newry arc into a genuine tri-hospital network under Option B.
- This completes NI’s coverage map: every population centre now within ~60 min of at least one fully staffed acute hospital.
Any downsides or caveats?
⚠️ Construction cost vs immediate health ROI — while the bridge/approach roads (~£250–300 m range depending on design) is primarily a transport project, health gains are indirect (saved travel time, staffing efficiency).
⚠️ Emergency network re-design required — ambulance dispatch protocols, hub assignments, and patient flow models would need to be re-mapped once the link opens.
⚠️ Environmental impact alignment — Option B and Sláintecare both stress sustainability; benefits are derived from reduced emissions from shorter emergency journeys and staff commuting outweighing new car flows.

The heart of the argument: not “who keeps an A&E” but “which hospital is actually built to deliver safe, sustainable care under Option B.”
Below is a full run of every hospital from the Option B dataset — Northern Ireland first, then Republic of Ireland — with a one-line ranking of its realistic strength in an all-island convergence model. The lens I’m using for “strength” is:
- Can it safely function as a 24/7 acute hub (ED, ICU, theatres, diagnostics, staffing depth)?
- Is it a high-value specialist centre that the island needs (e.g. paediatrics, maternity, ortho, trauma)?
- Or is it better as an elective / diagnostics / step-down satellite (day cases, planned surgery, rehab), helping to clear waiting lists efficiently?
For each, labels are:
- TIER 1 = Core 24/7 Acute Hub (keep as a main emergency + ICU site)
- TIER 1S = National / Regional Specialist Hub (paeds, maternity, transplant, orthopaedics, etc.)
- TIER 2 = Elective & Diagnostic Satellite / Medical Assessment Unit (MAU), not justified as full 24/7 ED but still strategically valuable
- TIER 3 = Low strategic acute value under Option B (i.e. would not carry unscheduled acute load; likely step-down / rehab only)
This is exactly the classification when someone says “is my hospital safe?”
NORTHERN IRELAND
Royal Victoria Hospital, Belfast
Strength: Flagship tertiary acute for NI (trauma, cardiac, neuro); deepest consultant base; full ICU.
Tier: TIER 1 (Core 24/7 Acute Hub)
Belfast City Hospital, Belfast
Strength: Major acute medicine, renal, cancer centre; strong specialist rosters; high throughput.
Tier: TIER 1 (Core 24/7 Acute Hub)
Mater Infirmorum Hospital, Belfast
Strength: Historically acute inner-city cover, now limited; struggles to justify standalone 24/7 rota when RVH and City exist minutes away.
Tier: TIER 2 (Elective / assessment / urgent care only, not full 24/7 ED)
Royal Belfast Hospital for Sick Children, Belfast
Strength: Only full-scale standalone paediatric acute/ICU in NI; paeds critical mass.
Tier: TIER 1S (Specialist Paediatric Hub)
Royal Jubilee Maternity Hospital, Belfast
Strength: High-risk maternity / neonatal intensive care serving the region; can’t be casually replicated.
Tier: TIER 1S (Specialist Maternity Hub)
Musgrave Park Hospital, Belfast
Strength: Orthopaedics, spinal, elective surgical throughput; gold for backlog clearance and hip/knee waiting lists.
Tier: TIER 1S (Specialist Elective Ortho Hub)
Ulster Hospital, Dundonald
Strength: South Eastern Trust’s main acute; modern ED and ICU capacity; recruitment base for a large commuter population.
Tier: TIER 1 (Core 24/7 Acute Hub)
Lagan Valley Hospital, Lisburn
Strength: Day surgery, minor injury/urgent care, medical assessment; struggles to sustain full acute rota.
Tier: TIER 2 (Satellite elective / diagnostics / MAU)
Downe Hospital, Downpatrick
Strength: Local unscheduled care / assessment; ideal as urgent-care & short-stay medical unit if the Strangford Lough Crossing happens and Portaferry becomes ~15 min away.
Tier: TIER 2 (Satellite urgent / assessment hub; not full 24/7 ICU)
Antrim Area Hospital, Antrim
Strength: Full ED/ICU; covers North/Mid Antrim and bleeds into greater Belfast load; proven 24/7 acute.
Tier: TIER 1 (Core 24/7 Acute Hub)
Causeway Hospital, Coleraine
Strength: Acute cover for Causeway Coast / north coast tourism belt; provides ED/medicine/ surgery to a dispersed population; keeps Ballycastle/Bushmills within ~60 min.
Tier: TIER 1 (Core 24/7 Acute Hub, rural coverage argument)
Mid Ulster Hospital, Magherafelt
Strength: Medical assessment / limited inpatient beds; staffing depth for 24/7 full acute is not there; best use is step-down and rapid assessment.
Tier: TIER 2 (Assessment / step-down satellite)
Whiteabbey Hospital, Newtownabbey
Strength: Elective / rehab / recovery capacity close to Belfast headcount; extremely useful for clearing lists without tying up main theatres.
Tier: TIER 2 (Elective / rehab satellite)
Craigavon Area Hospital, Craigavon
Strength: Full-fat acute hub for the Southern Trust; critical for ABC / Portadown / Lurgan / Armagh / upper Bann; ICU, surgery, ED, diagnostics.
Tier: TIER 1 (Core 24/7 Acute Hub)
Daisy Hill Hospital, Newry
Strength: Acute ED and surgery with strong border catchment; natural link to Dundalk; essential to the Down- Newry-Dundalk spine.
Tier: TIER 1 (Core 24/7 Acute Hub)
South Tyrone Hospital, Dungannon
Strength: Day surgery, endoscopy, assessment; not realistic to sustain full ED/ICU rota independently of Craigavon.
Tier: TIER 2 (Elective/day-case satellite)
Altnagelvin Area Hospital, Derry/Londonderry
Strength: West-of-the-Bann tertiary acute including oncology centre and cross-border service into Donegal; very high strategic value.
Tier: TIER 1 (Core 24/7 Acute Hub)
South West Acute Hospital, Enniskillen
Strength: Modern build, ICU-capable, remote coverage for Fermanagh/SW; vital to keep 24/7 because travel times are brutal otherwise.
Tier: TIER 1 (Core 24/7 Acute Hub)
Omagh Hospital & Primary Care Complex, Omagh
Strength: Urgent care, diagnostics, day surgery; too close to Enniskillen and Altnagelvin to justify full ICU/ED overnight; perfect spoke.
Tier: TIER 2 (Satellite urgent / diagnostic hub)
NI summary:
- TIER 1 (Core Acute Hubs): RVH, Belfast City, Ulster, Antrim, Causeway, Craigavon, Daisy Hill, Altnagelvin, South West Acute
- TIER 1S (Specialist Only): Royal Belfast for Sick Children, Royal Jubilee Maternity, Musgrave Park
- TIER 2 (Elective / Assessment Satellites): Mater, Lagan Valley, Downe, Mid Ulster, Whiteabbey, South Tyrone, Omagh
- TIER 3: none in NI list — everything kept in some role
That is your NI network under Option B.
REPUBLIC OF IRELAND
(Dublin region first, then rest by group)
Beaumont Hospital, Dublin
Strength: Neurosurgery, transplant, ICU depth, ED volume, tertiary.
Tier: TIER 1 (Core 24/7 Acute Hub)
Mater Misericordiae University Hospital, Dublin
Strength: Tertiary acute with cardiac, ICU, complex surgery; national specialties.
Tier: TIER 1 (Core 24/7 Acute Hub)
St James’s Hospital, Dublin
Strength: Ireland’s biggest adult acute/tertiary teaching hospital; high-level oncology, ICU, trauma.
Tier: TIER 1 (Core 24/7 Acute Hub)
St Vincent’s University Hospital, Dublin
Strength: Tertiary centre with transplant/hepatobiliary; major ED; specialist rosters.
Tier: TIER 1 (Core 24/7 Acute Hub)
Tallaght University Hospital, Dublin 24
Strength: Full ED/ICU for SW Dublin / Kildare belt; stepwise capacity for overflow; strong general surgery/medicine.
Tier: TIER 1 (Core 24/7 Acute Hub)
Connolly Hospital, Blanchardstown
Strength: ED/acute medical/surgical and ICU serving west Dublin / Meath; valuable workforce base.
Tier: TIER 1 (Core 24/7 Acute Hub)
National Orthopaedic Hospital Cappagh, Dublin
Strength: Dedicated high-volume orthopaedic elective centre; absolutely critical for waiting list burn-down.
Tier: TIER 1S (Specialist Elective Surgical Hub)
Coombe Women & Infants University Hospital, Dublin
Strength: Complex maternity and neonatal intensive care.
Tier: TIER 1S (Specialist Maternity Hub)
National Maternity Hospital (Holles Street), Dublin
Strength: National referral maternity; high-risk obstetrics.
Tier: TIER 1S (Specialist Maternity Hub)
Rotunda Hospital, Dublin
Strength: Maternity & neonatal with deep staffing pool; historic national role.
Tier: TIER 1S (Specialist Maternity Hub)
Children’s Health Ireland at Crumlin
Strength: Full paediatric tertiary (surgery, cardiac, ICU).
Tier: TIER 1S (Specialist Paediatric Hub)
CHI at Temple Street
Strength: Paediatric acute/ED (neuro, ENT etc. historically), transitioning into the new national children’s model.
Tier: TIER 1S (Specialist Paediatric Hub)
CHI at Tallaght / Connolly
Strength: Paediatric urgent / day-case; relieves pressure off main paeds tertiary; improves access outside city centre.
Tier: TIER 1S (Specialist Paediatric Satellite Hub)
Our Lady of Lourdes Hospital, Drogheda (Louth)
Strength: Full ED/ICU; main acute hub for Louth/Meath/Northeast; critical cross-border interface with Newry/Daisy Hill.
Tier: TIER 1 (Core 24/7 Acute Hub)
Our Lady’s Hospital Navan (Meath)
Strength: Politically sensitive; limited ability to sustain full 24/7 rota; realistically becomes medical assessment and urgent care, not full trauma.
Tier: TIER 2 (MAU / limited unscheduled, not full acute hub)
Louth County Hospital, Dundalk
Strength: Assessment unit / injuries / day surgery; not viable for full ICU/ED rosters.
Tier: TIER 2 (Satellite elective / assessment)
Midland Regional Hospital Tullamore (Offaly)
Strength: Acute surgery, ICU, ED; anchors Midlands.
Tier: TIER 1 (Core 24/7 Acute Hub)
Midland Regional Hospital Mullingar (Westmeath)
Strength: Acute general hospital with ED; critical Midlands coverage.
Tier: TIER 1 (Core 24/7 Acute Hub)
Midland Regional Hospital Portlaoise (Laois)
Strength: Has struggled to retain full 24/7 profile; maternity already politically contested; clinically safer future as high-throughput assessment + day surgery.
Tier: TIER 2 (Satellite MAU / planned care)
St Luke’s General Hospital, Kilkenny
Strength: Acute ED / general surgery / medicine for Carlow-Kilkenny; consistent staffing argument.
Tier: TIER 1 (Core 24/7 Acute Hub)
University Hospital Galway
Strength: Western tertiary hub: neurosurgery, cardiac, ICU depth; pulls all of Connacht and part of the Midlands.
Tier: TIER 1 (Core 24/7 Acute Hub)
Merlin Park Hospital, Galway
Strength: Elective ortho / rehab / step-down capacity for Galway; crucial to clearing surgical backlogs without clogging Galway UHG theatres.
Tier: TIER 1S (Specialist Elective Hub)
Mayo University Hospital, Castlebar
Strength: Acute ED/ICU for Mayo. Geographically essential because West/Northwest distances are brutal.
Tier: TIER 1 (Core 24/7 Acute Hub)
Sligo University Hospital
Strength: Acute ED/ICU for Sligo/Leitrim/NW; also backs cross-border Donegal patients when Letterkenny is pressured.
Tier: TIER 1 (Core 24/7 Acute Hub)
Letterkenny University Hospital, Donegal
Strength: Acute ED/ICU for Donegal; absolutely non-negotiable given isolation.
Tier: TIER 1 (Core 24/7 Acute Hub)
Portiuncula University Hospital, Ballinasloe
Strength: Mixed medicine/surgery/ED for East Galway / South Roscommon; valuable to keep throughput out of Galway City.
Tier: TIER 1 (Core 24/7 Acute Hub)
Roscommon University Hospital
Strength: Reconfigured years ago away from full 24/7 ED; functions as MAU / day surgery / diagnostics; politically sensitive but clinically already Tier 2 profile.
Tier: TIER 2 (Satellite elective / assessment)
University Hospital Limerick
Strength: Only 24/7 ED for the UL Hospitals Group; overloaded but strategically essential; ICU, surgery, trauma.
Tier: TIER 1 (Core 24/7 Acute Hub)
Ennis Hospital, Clare
Strength: Medical assessment, day surgery, injuries; cannot sustain full ICU/ED autonomously; acts as pressure valve for Limerick.
Tier: TIER 2 (Satellite MAU / elective)
Nenagh Hospital, North Tipperary
Strength: Day surgery, diagnostics, medical assessment; similar profile to Ennis.
Tier: TIER 2 (Satellite MAU / elective)
St John’s Hospital, Limerick (city)
Strength: Sub-acute medical/surgical capacity that relieves UHL inpatient pressure; incredibly valuable as planned-care spillover in a system with chronic overcrowding.
Tier: TIER 2 (Urban elective / step-down satellite)
Cork University Hospital, Cork
Strength: Southern tertiary / major trauma / ICU depth / complex surgery; irreplaceable for Munster.
Tier: TIER 1 (Core 24/7 Acute Hub)
Mercy University Hospital, Cork
Strength: City-centre acute cover, ED, general medicine/surgery; supports CUH load.
Tier: TIER 1 (Core 24/7 Acute Hub)
South Infirmary Victoria University Hospital, Cork
Strength: Elective surgical (ENT, plastics, ortho subspecialty); crucial high-throughput elective hub.
Tier: TIER 1S (Specialist Elective Surgical Hub)
Cork University Maternity Hospital, Cork
Strength: Regional maternity / neonatal intensive care for Cork & Kerry.
Tier: TIER 1S (Specialist Maternity Hub)
Mallow General Hospital, North Cork
Strength: MAU, injuries, some short-stay medical; not viable as standalone 24/7 ICU/ED.
Tier: TIER 2 (Rural satellite / assessment)
Bantry General Hospital, West Cork
Strength: Remote coastal cover, stabilisation, injuries, elderly care; struggle to staff full ED, but lifesaving as a stabilise-and-transfer node.
Tier: TIER 2 (Remote satellite / urgent-stabilise)
University Hospital Kerry, Tralee
Strength: Full ED/ICU for Kerry; distance from Cork means it must stay Tier 1.
Tier: TIER 1 (Core 24/7 Acute Hub)
University Hospital Waterford
Strength: Acute ED/ICU + cardiac services for Waterford / South East; growing regional cardiac centre.
Tier: TIER 1 (Core 24/7 Acute Hub)
Wexford General Hospital, Wexford
Strength: Acute general hospital for Wexford; obstetrics and emergency general surgery; important for the South East, distance to Waterford.
Tier: TIER 1 (Core 24/7 Acute Hub)
Tipperary University Hospital (Clonmel)
Strength: Acute ED/ICU, surgery, maternity for South Tipp / East Munster; high value because South Tipp is too far to be safely absorbed entirely into Cork or Waterford.
Tier: TIER 1 (Core 24/7 Acute Hub)
St Luke’s / “University Hospital Kilkenny” (Kilkenny)
Strength: Acute ED/surgery internal to Carlow-Kilkenny cluster; strong generalist staffing base.
Tier: TIER 1 (Core 24/7 Acute Hub)
(“Kilcreene” orthopaedic in Kilkenny wasn’t listed separately in our planning sheet, but that functions like Cappagh/Merlin Park: high-value elective ortho. It’s structurally Tier 1S when it’s operating as a dedicated high-throughput elective unit.)
ROI summary:
- TIER 1 (Core 24/7 Acute Hubs): Beaumont, Mater, St James’s, SVUH, Tallaght, Connolly, Drogheda, Tullamore, Mullingar, Kilkenny, Galway UHG, Mayo, Sligo, Letterkenny, Portiuncula, Limerick UHL, CUH Cork, Mercy Cork, Kerry (Tralee), Waterford, Wexford, Clonmel (Tipperary UH)
- TIER 1S (Specialist Hubs): Cappagh, Coombe, NMH, Rotunda, CHI Crumlin, CHI Temple Street, CHI Tallaght/Connolly, Merlin Park, South Infirmary Victoria, Cork University Maternity (and Kilcreene-type ortho if separated)
- TIER 2 (Satellite MAU / Elective / Day Surgery / Step-down): Navan, Louth County (Dundalk), Portlaoise, Roscommon, Ennis, Nenagh, St John’s (Limerick), Mallow, Bantry
- TIER 3: none; every site has defined future function
––––––––––––
HOW TO READ THIS POLITICALLY
––––––––––––
- A “closure” under Option B is almost never an actual physical shutdown.
It is: “You are no longer pretending to be a full 24/7 ICU/ED hospital. You are now a high-throughput planned-care / diagnostic / assessment centre to cut waiting lists and keep frail patients close to home.” - Tier 2 hospitals (Lisburn, Downe, Bantry, Ennis, etc.) become the pressure valves that stop the Tier 1 hubs from drowning.
This is how you cut waiting lists without needing to build 10 new megahospitals. - Tier 1S specialist hubs (paediatric, maternity, orthopaedics, transplant) are untouchable.
They are not “small hospitals” — they are the reason you don’t have to duplicate rare, expensive, high-risk services everywhere. - If you ever have to defend the plan publicly:
- “No community loses a hospital.”
- “Every hospital gets a defined clinical role.”
- “But only those hospitals that can actually sustain 24/7 emergency medicine + ICU + surgical cover will keep doing that.”
Closing Paragraph
Health reform is not about closing hospitals — it is about connecting them.
The Bengoa Report gave Northern Ireland the framework; Option B now gives the island the roadmap.
But unless we deal with geography, the best plans will keep failing at the water’s edge.
The Strangford Lough Crossing is the missing link that unites the South Eastern and Southern Trusts into one continuous emergency and elective network — allowing Downe, Daisy Hill, and Ulster Hospital to function as partners, not competitors.
For MLAs who have fought for their local hospitals, this is the practical way to secure them: make them accessible, share their workloads, and embed them within an all-island system that guarantees the same standard of care for every patient, north or south.
Supporting the SLC is therefore not a diversion from healthcare reform — it is the decisive act that finally makes Bengoa deliverable.

